India’s Health Sub-Center Crisis: How Digital Health Records Can Bridge the Rural Care Gap
A Rural Healthcare Wake-up Call
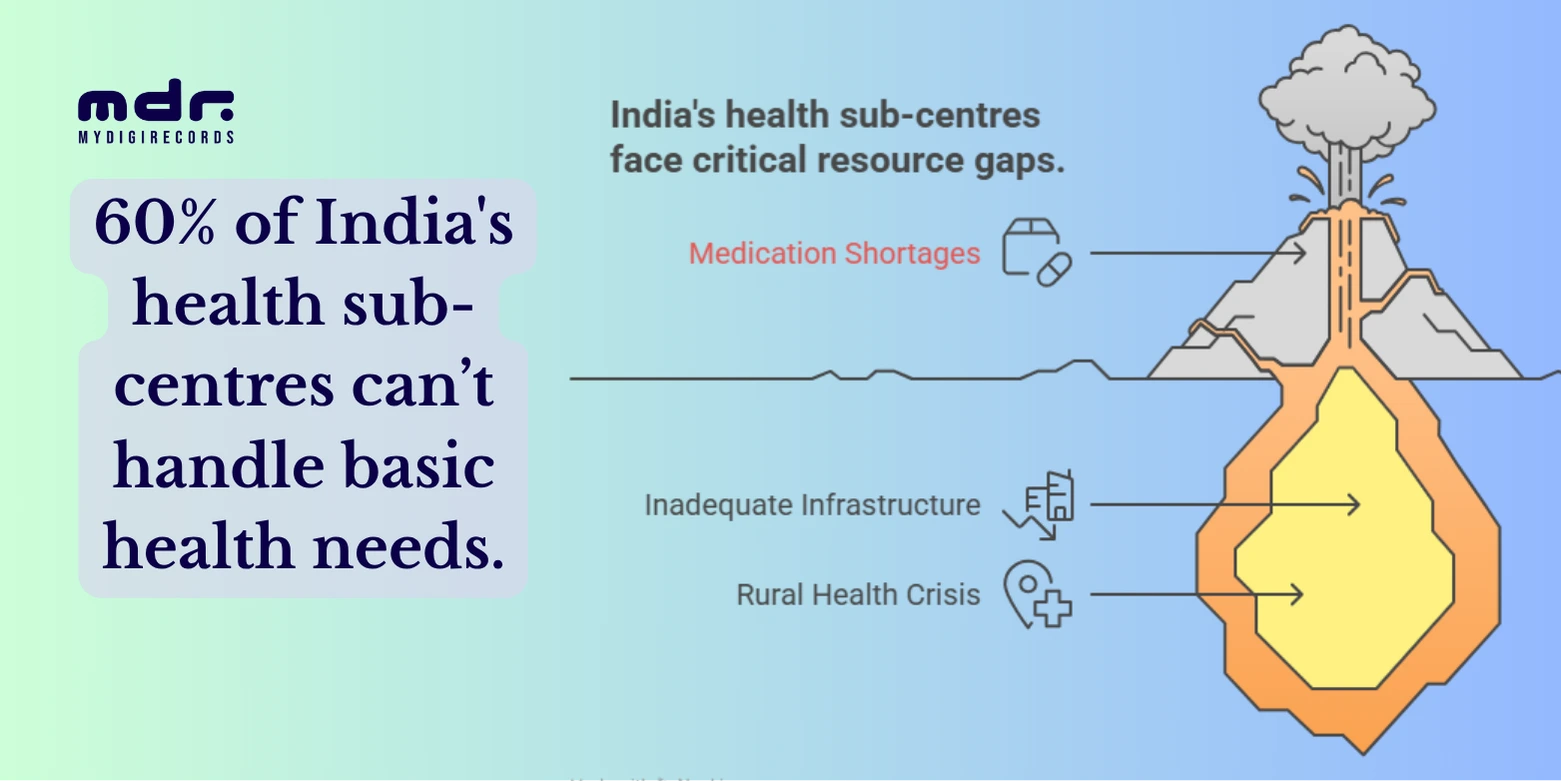
A recent nationwide survey has delivered a jarring verdict: 60% of India’s rural health sub-centers – the most basic units in the public health delivery system – are unable to manage common yet life-threatening conditions like diabetes and hypertension.
For a country that boasts one of the largest healthcare infrastructures on paper, this finding underscores a major disparity between infrastructure and impact. These sub-centers are the first point of care for nearly 69% of India’s rural population, yet they’re falling behind in addressing even the most fundamental health needs.
In this blog, we explore the data, impact, and a way forward – centered on digital health innovations like MyDigiRecords (MDR) that can empower frontline healthcare workers and improve patient outcomes, especially in underserved rural areas.
Also Read: Best PHR App: MyDigiRecords (MDR) | Your Ultimate Health Companion
The Data Behind the Crisis
Let’s unpack the key findings from the survey:
Key Indicator | Statistic |
Sub-centers unable to manage BP, diabetes | 60% |
Population served by each sub-center | 5,000 (plain areas) / 3,000 (tribal) |
No functional diagnostics in majority | 70%+ |
Shortage of male health workers | 65% vacant posts |
Percentage of IPHS-compliant sub-centers | <4% |
Why This Is More Than Just a Rural Problem
Although the issue is rooted in rural infrastructure, its consequences are national:
- Delayed Diagnoses: Without early detection of hypertension or diabetes, patients reach hospitals at advanced stages, increasing mortality risks.
- Hospital Overcrowding: Sub-centers failing to treat leads to unnecessary burden on Primary Health Centers (PHCs) and district hospitals.
- Healthcare Cost Surge: Out-of-pocket expenses rise as patients turn to private providers due to poor public health access.
Digital Divide: Lack of health records means patients cannot carry or share past diagnoses, worsening treatment continuity.
Root Causes: What’s Going Wrong?
1. Infrastructure Gaps
Despite India’s ambitious health programs, ground-level infrastructure hasn’t kept pace:
- Absence of electricity, running water, or dedicated buildings in some regions.
- Poor maintenance of existing equipment and buildings.
- Lack of essential diagnostics.
2. Human Resource Shortage
- Many sub-centers have only one ANM (Auxiliary Nurse Midwife) managing multiple villages.
- Posts for male health workers remain vacant in most states.
- Overwork leads to absenteeism, burnout, and sub-par care.
3. Manual Records & Data Silos
- No digital tracking of patients’ vitals, medication, or chronic conditions.
- Sub-centers operate in isolation—data doesn’t travel to PHCs or state-level systems.
Zero analytics on which conditions are rising, where, and among whom.
The Role of Technology: Can Digital Health Records Help?
Yes—and that’s where MyDigiRecords (MDR) steps in.
What is MDR App?
MyDigiRecords is a smart health record platform that lets patients and healthcare  providers digitally create, access, and share personal health records, including:
providers digitally create, access, and share personal health records, including:
- Blood pressure readings
- Hydration levels
- Heart Rate
- Medication history
- Immunization and screening data
- AI-based health trend predictions
For sub-centers with limited resources, MDR acts as a plug-and-play health assistant, enabling accurate data capture, continuity of care, and population-level health monitoring.
Also Read: How Digital Health Records Simplify Your Life in 2025
How MDR Can Solve the Sub-Center Crisis
1. Digitizing Patient Records at the Point of Care
Even if diagnostic tools are available, manual records are often lost or poorly maintained. MDR lets ANMs and ASHA workers:
- Log vitals using their smartphones or tablets.
- Track blood pressure or heart rate, hydration levels for individuals over time.
- Flag high-risk patients early for referrals.
2. Offline Sync for Remote Areas
In areas with poor internet, MDR works offline-first and syncs data automatically when the connection returns. This ensures rural sub-centers stay digitally connected without network dependency.
3. Empowering ASHAs and ANMs
- ASHA workers can carry patient QR codes for scanning and updating.
- Access previous reports, vaccination logs, and medication history in seconds.
- Eliminate duplicate testing or treatment errors.
4. Creating a Population Health Map
With aggregated, anonymized data:
- Health departments can identify villages with rising BP/diabetes cases.
- Plan targeted screening camps or medicine distribution.
- Track vaccination dropouts or maternal health alerts.
5. Government Integration Possibilities
India has already launched ABHA (Ayushman Bharat Health Account) and the NDHM (National Digital Health Mission). MDR can integrate seamlessly with these by:
- Generating ABHA-linked records.
- Contributing data to Health IDs.
- Helping rural patients carry their entire health history in their phone or QR code—even if they move to another city or state.
What Needs to Happen Next
For Policymakers:
- Mandate digital health record systems like MDR at all sub-centers.
- Invest in mobile devices for ASHA/ANM workers.
- Align MDR integration with Ayushman Bharat’s digital health goals.
For NGOs & Public Health Projects:
- Partner with MyDigiRecords to roll out region-wide pilot programs.
- Train healthcare workers in basic digital literacy.
- Leverage data dashboards to drive community health planning.
For Citizens:
- Encourage rural families to adopt MDR for tracking their health records.
- Empower local youth or SHGs to assist ANMs in recordkeeping.
Conclusion: Digitization is the Vaccine for Rural Healthcare Gaps
The 60% failure rate of sub-centers to handle basic care is alarming, but not unsolvable.
With health tools like MyDigiRecords, even the remotest sub-centers can be transformed into data-smart health nodes – capable of early detection, digital continuity, and efficient public health response.
This isn’t about replacing doctors or workers—it’s about empowering them.
As India continues its digital transformation, bringing the power of health data to rural frontlines must be a priority. Because in a nation of 1.4 billion, every heartbeat—and every blood pressure reading – counts.
More blogs for you to read
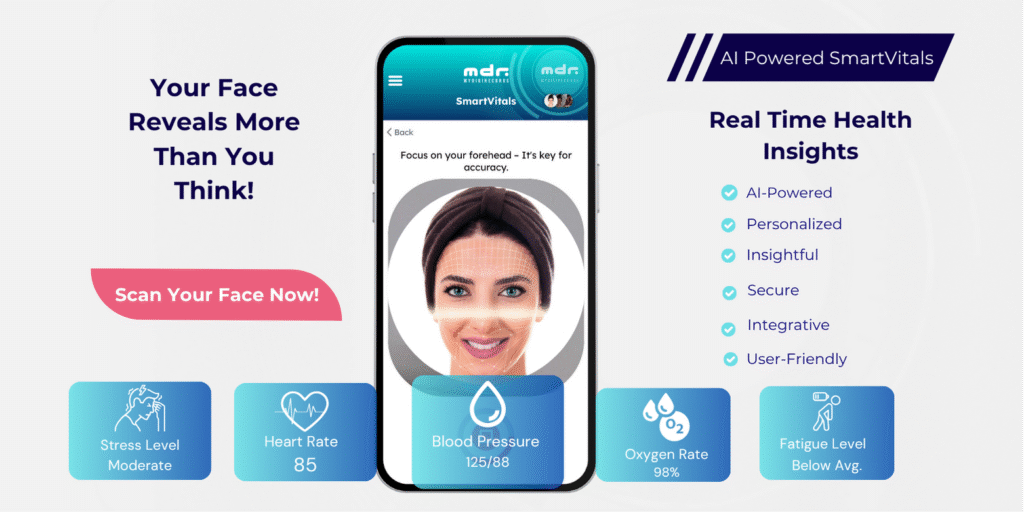
AI-Powered Face Scan: The Future of Blood Pressure Monitoring Is Here
AI-Powered Face Scan: The Future of Blood Pressure Monitoring Is Here Table of Contents: Introduction The Rise of Contactless Health

How Smart Clinics Are Using AI to Speed Up Diagnosis and Treatment
How Smart Clinics Are Using AI to Speed Up Diagnosis and Treatment Table of Contents: Introduction What Are Smart Clinics?

Vaccination Vault: Why Keeping Digital Records Is Now a Must in 2025
Vaccination Vault: Why Keeping Digital Records Is Now a Must in 2025 Table of Contents: Introduction Why Vaccine Records Matter

From Allergies to Emergencies: How Digital Records Can Save Children’s Lives
From Allergies to Emergencies: How Digital Records Can Save Children’s Lives Table of Contents: Why Every Second Matters The Hidden

Managing Medicines for the Whole Family? Here’s How to Do It with One App
Managing Medicines for the Whole Family? Here’s How to Do It with One App Table of Contents: Introduction Why Medication

How Corporates Can Use AI-Powered Health Data to Boost Productivity
How Corporates Can Use AI-Powered Health Data to Boost Productivity Table of Contents: Introduction The Rise of AI in Corporate
Top Health Tracking App in 2025: Introducing SmartVitals — Track Heart Rate, Blood Pressure, Sleep & More in One Place
Top Health Tracking App in 2025: Introducing SmartVitals – Track Heart Rate, Blood Pressure, Sleep & More in One Place

The Hidden Risks of Poor Health Record-Keeping in Schools – And Why Digitalization Is the Way Forward
The Hidden Risks of Poor Health Record-Keeping in Schools – And Why Digitalization Is the Way Forward Table of Contents:
Smart Travel, Smarter Health: How AI is Personalizing Your Next Trip
Smart Travel, Smarter Health: How AI is Personalizing Your Next Trip Table of Contents: Introduction The Evolution of Travel: From

Prenatal Care App: The Must-Have Tool for Every Mom-to-Be
The Must-Have Tool for Every Mom-to-Be: Prenatal Care App – A Smart Move for a Healthy Journey Table of Contents:

